Ali Amra
Professor Shermak
Com 102-054
3rd, May 2013
Technological Advances Aiding the Treatment of Oral Cancer
Cancer is a disease in which cells divide uncontrollably, which leads to the formation of tumors. It is the most despised disease anyone would want to be diagnosed with, because it currently has no found cure. According to the National Cancer Institute at the National Institutes of Health, oral cancer forms in the oropharynx, or the oral cavity. “The ratings of oral cancer in 2013 are 41,380 cases and 7,890 deaths.” (National Cancer Institute). These stats are very high in frequency per year just for one type of cancer. “As of 2004, oral cancer is the 6th leading cause of cancer deaths.” (Osuna and Hopkins, 2008) According to the Illinois Department of Public Health, “According to the Illinois State Cancer Registry, about 1,480 new cases of oral and pharyngeal cancer will be diagnosed in Illinois in 2008.” (Illinois Department of Public Health)
“In the past 40 years, there have been tremendous improvements in oral cancer care.” (Dr. Song, 2008) According to Dr. Song, 2008, despite the advances in oral cancer care, the government and scientists are focusing and funding more for the treatment of more common cancers, such as breast and lung cancer, rather than oral cancer. “Overall, 60% of people with oral cancer survive for 5 years.” (National Institute of Dental and Craniofacial Research) Despite the lower survival rate of oral cancer, physicians like Dr. Song are trying to gain awareness about oral cancer because this disease is not being funded to go under study.
Oral cancer is one of the most fatal cancers because it has relatively low survival rates. If oral cancer is diagnosed late, the likelihood of survival is rare, which is disappointing because a diagnosed patient can do his utmost to survive, but will most likely fail to do so. Despite paying large sums of money and going through numerous medical processes to treat oral cancer, the disease continues to progress to fatal stages. Despite the extreme advances in technology, the cure for cancer has yet to have been found. However, many methods to find a cure and more effective treatments are being studied, practiced and introduced by scientists today. These methods vary in strategies, but all of them have one objective, which is to treat and cure oral cancer effectively. Some of these methods include: surgery, lab on a chip technology, molecular level approaches and radiation therapy.
Surgery for oral cancer involves, removing tumors in tissues to minimize the amount of cancerous cells. “Many oral cancer surgery patients are often concerned about disfigurement; but recent advances in reconstructive surgery mean that appearances can be restored, sometimes with little or no change.” (Cancer Treatment Centers of America) Completing these surgical processes depend on the patient’s stage of oral cancer. As stated by the Cancer Treatment Centers of America, removing tumors from oral cancer through surgery includes various surgical techniques. Some of these techniques include tumor resection and gastrostomy.
Tumor resection is “An operation to remove the entire tumor.” (Cancer Treatment Centers of America) This surgical process can lead to the maxillary defects of the affected region. The Department of Oral Maxillofacial surgery at Marma University states that, a newly introduced technology, 3D screening, can be used to help minimize the loss of normal cells during resection process. They also stated that the 3D screening can also be used to ensure the safety of reconstructive process which includes the implanting of zygoma to replace lost tissues. “In particular, before zygoma implant placement, 3D imaging and planning should be performed to ensure the safety of surgery and rehabilitation.” (Ugurlu, Yildiz, Sener, and Sertgoz, 2013)
“Gastrostomy tube is a feeding tube that can be inserted directly into the stomach.” (Cancer Treatment Centers of America) According to the Cancer Treatment Centers of America, this method should only be used if oral cancer is preventing swallowing. This process consists of a tube that can easily be inserted through the mouth into the stomach, to ensure the patient’s nutrition. The tube can also be removed easily once nutrition returns to its norm. “A camera is attached to the end of a long thin tube, allowing your doctor to see directly into the stomach.” (Cancer Treatment Centers of America) This camera allows the doctor to know that the tube is functioning correctly.
Another method that is used to improve the treatment for oral cancer is the lab on a chip technology. “The chip is based on determining a 30-gene transcription profile in cancer cells isolated from fluid samples.” (Haim, Zobier, Chen, Mauk and Thompson, 2007) This technological development is beneficial for treating oral cancer because it can prevent complex surgical procedures that lead to disfigurement. According to the article, surgical procedures are the last resort to treating oral cancer during it’s the late stages. “Early detection of OSCC (Oral squamous cell carcinoma) could greatly reduce morbidity by fostering more timely initiations of therapy and patient monitoring, and also would help avoid inappropriately aggressive surgical treatments that result in severe disfigurement.” (Haim, Zobier, Chen, Mauk and Thompson, 2007) As stated by the authors, the lab on a chip microfluidics allows dentists and doctors to easily screen oral cancer without extensive training. This method is advantageous to the patients because it is inexpensive, speedy, and its efficient ability to detect oral cancer at its early stages.
Molecular level approaches help treat oral cancer by using the method of trying to prevent it. “The genomic era has fueled a rapid emergence of new information at the molecular level with a great potential for developing innovative approaches to detection, risk assessment, and management of oral cancers and premalignant disease.” (Rosin, Poh, Guillard, Williams, Zhang and MacAulay, pg. 167) According to the authors, this method has gone through an eight year practice to finally correlate with the patient outcome. “The plan is to use step-by-step sequence to guide clinicopathological on patient risk and treatment.” (Rosin, Poh, Guillard, Williams, Zhang and MacAulay, pg. 167) Some of the technologies that are used in this procedure are, the hand held visualization which is basically used to detect abnormal lesions. Then 2 computer systems, called microscopy systems are used to the measure protein expression of the cell’s phenotype, which is the expressed trait of the cell.
According to the authors, over the past 10 years radiation therapy has evolved to efficiently treat cancer by kill cancer cells, including oral cancer. This is because of the technological advancements in radiotherapy. “Technical improvements in the application of x-rays, computed tomography scans, magnetic resonance imaging with and without spectroscopy, ultrasound, positron emission tomography scans, and electronic portal imaging—and our understanding of their limitations— have greatly improved our ability to identify tumors.” (Bucci, Bevan, and Roach pg. 117) As stated by the authors, back then radiotherapy was in 2D, which only consisted of one to four beams. More recently, the 3D radiotherapy was introduced and effectively used to approximately measure irregular shapes. “While 3D planning allowed for accurate dose calculations to such irregular shapes, we were still limited in the corrections we could make.”(Bucci, Bevan, and Roach pg. 118) Therefore, the 3D radiation therapy improved to IMRT, which is Intensity modulation radiation therapy. This therapy allows for certain beam to work under high intensity while others are at lower intensities. The reason for different intensity level beams allowed for more dosage control. Further developments of radiotherapy led to the progress of IMRT to 4D therapy. These improvements took place because 3D and IMRT therapy changes the patient’s anatomy, which meant new calculations need to be considered. “The next direction in radiation oncology is to account for this movement and is being called four-dimensional (4D) conformal radiotherapy (CRT), a logical progression from 3D CRT.” (Bucci, Bevan, and Roach pg. 118) The 4D therapy uses a megavoltage coned beam to dose the patient based on the patient’s current anatomy.
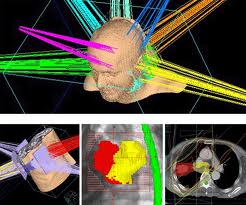
This photo portrays the 3D radiotherapy used to treat cancers including oral cancer. It shows how technology changed, by illustrating the efficient beams that target all angles of the neck and head. The new angles of beams allow radiotherapy to kill cancerous cells proficiently.
Oral Cancer Screening San Diego VELscope Provider Visual Enhanced Lesion Scope Technology:
This video advertises the new efficient technology created. This technology is used to detect oral cancer at its early stages. Detecting oral cancer early can increase the possibility of being cured. As stated in the video, the VELscope can detect oral areas that have the potential to become cancerous. According to Dr. Jen Kim, “The Velscope’s blue light “excites” molecules (called “fluorophores”) deep within the layers of oral mucosal tissues.” (Dr. Kim, Jen Kim Dentistry) This allows doctors or dentists to differentiate between normal and abnormal cells.
Over time technology has evolved to effectively aid the treatment for oral cancer. Many technologies were created over the past years which helped improve the treatment of this fatal disease. Although, the technologies differed in strategies each technology continues to play an important role in the treatment of this type of cancer. These methods included are surgery, lab on a chip technology, molecular level approaches, and radiation therapy. As technology aiding the treatment for oral cancer continues to progress, one can only imagine what types of technology will be used in the future to treat this deadly disease that has killed many people throughout the years.
References:
Bucci, M. , Bevan Alison. and Roach, Mark. “Advances in Radiation Therapy: Conventional to 3D, to IMRT, to 4D, and Beyond” Department of Radiation Oncology. San Francisco, March 2005: 117-134. Web. 2 May. 2013
Calum MacAulay, et al. “Visualization and Other Emerging Technologies as Change Makers For Oral Cancer Prevention.” Annals of the New York Academy Of Sciences 1098.(2007): 167-183. Academic Search Complete. Web. 7 Apr. 2013.
Dentist92115. “Oral Cancer Screening San Diego VELscope Provider Visual Enhanced Lesion Scope Technology” Online Video Clip. YouTube. You Tube, 24 May. 2012. Web 5 May. 2013
Haim H. Bau, et al. “Lab-On-A-Chip Technologies for Oral-Based Cancer Screening and Diagnostics” Annals of the New York Academy of Sciences 1098. (2007): 467-475. Academic Search Complete. Web. 7 Apr. 2013
Jen, Kim. “How Does the Velscope Work?” Jen Kim Dentistry FAQs. Web. 5 May. 2013
National Cancer Institute at the National Institutes of Health. “Oral Cancer.” National Cancer Institute. Web. 2 May. 2013
Osuna, Tricia and Hopkins, Suzie. “Oral Cancer Diagnostic Technologies” CDHA Journal Vol. 24 No. 1. (2008): 12-17. Web. 2 May. 2013
Song, John. “Is Oral Cancer More Deadly Than Other Cancers?” Ed Zimney. (2008.) Web. 2 May. 2013
Urglu, Faysal. , Yildiz, Coskun. , Sener. and Atilla. “Rehabilitation of Posterior Maxilla with Zygomatic and Dental Implant After Tumor Resection: A Case Report” Case Reports in Dentistry. (2013.) Web. 2 May. 2013
